Pyruvate Kinase Deficiency ( PKD) is an uncommon heritable metabolic condition performing in habitual hemolytic anemia, caused by mutations of the PKLR gene which encodes for the pyruvate kinase enzyme responsible for producing energy within red blood cells; lack of this enzyme causes red blood cells to break down precariously leading to anemia, hostility, gallstones, and fresh complications.
Bone marrow Transplant( BMT), also referred to as Hematopoietic Stem Cell Transplantation( HSCT), remains the only known restorative remedy for Polycythemia Vera Diseases( PKDs), still, this comes with pitfalls and challenges of its own. This blog explores the potential advantages and drawbacks of BMT/HSCT as a treatment option for PKD patients.
Understanding Pyruvate Kinase Deficiencies
PKD interferes with the red blood cell’s ability to produce Adenosine Triphosphate, or ATP, an essential energy source needed by cells for proper functioning. Without enough ATP production, red blood cells become fragile and break down too rapidly leading to hemolytic anemia and chronic anemia; with symptoms including:
- Fatigue and weakness
- Jaundice( yellowing of the skin and eyes).
- Blowup of the Spleen( Splenomegaly)
- Gallstones
- Growth Detainments in Children
While probative curatives like blood transfusions, folic acid supplementation, and surgical junking of the spleen( known as splenectomy) may give short-term relief, they don’t address the root cause; bone marrow transplantation offers hope in curing this illness.
What Is Bone Marrow Transplantation?
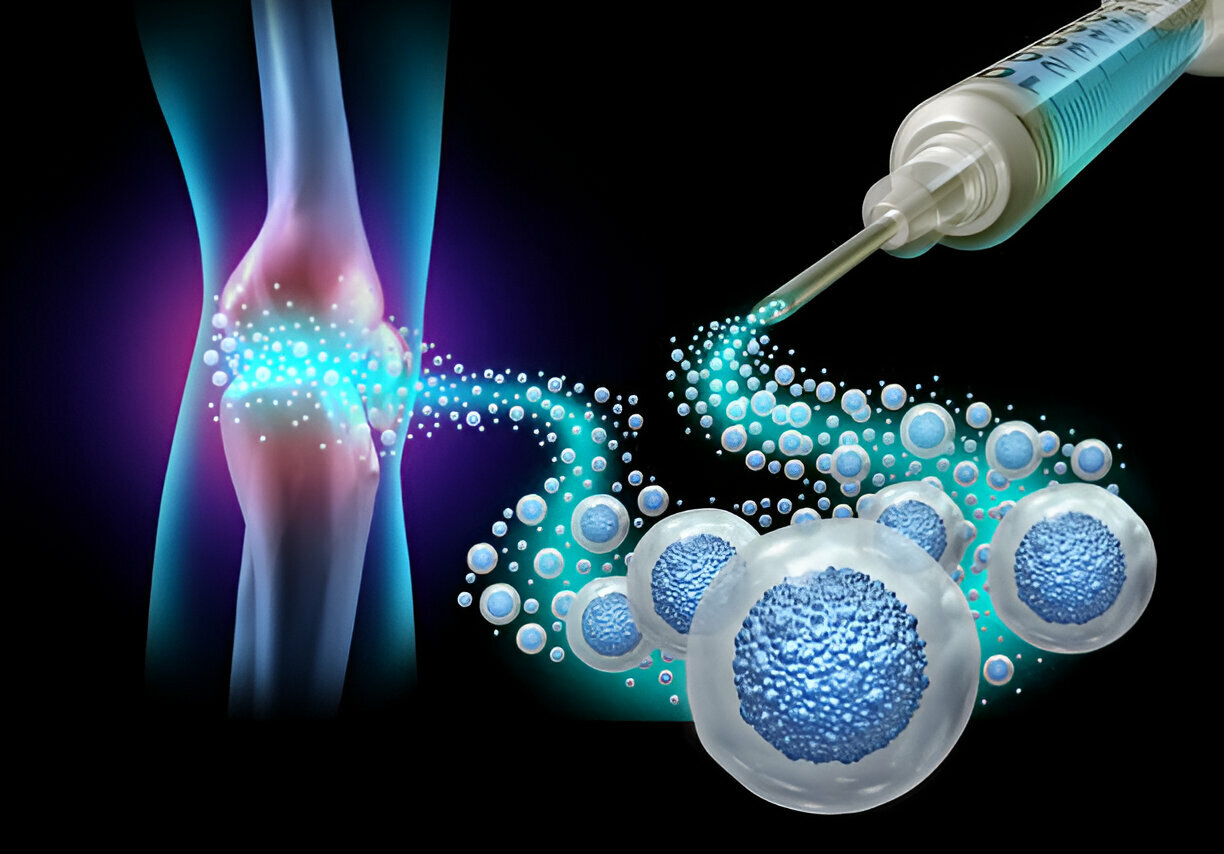
Bone marrow transplantation involves replacing damaged bone marrow( that produces abnormal red blood cells) with healthy stem cells from a patron, so they can develop into normal red blood cells with completely functional pyruvate kinase enzymes and give relief to any associated diseases.
Bone marrow transplants come in two primary kinds.
- Autologous Transplantation – To treat PKD, stem cells collected, treated and then reincorporated from another person are taken, though this option would leave genetic defects uncorrected.
- Allogeneic Transplantation – Stem cells from compatible donors (usually siblings or unrelated unrelated donors ) may be taken to replace damaged bone marrow in patients.
As PKD is an inherited disorder, an allogeneic transplant must take place to provide healthy stem cells capable of producing normal red blood cells.
Benefits of Bone Marrow Transplant for Patients of PKD.
1. Potential Cure
The primary benefit of BMT lies in its potential cure for PKD. After receiving healthy stem cells, bone marrow begins producing fully functional red blood cells on its own and doesn’t need additional transfusions and supportive treatments indefinitely.
2. Decrease Need for Transfusions
Numerous patients with PKD require regular blood transfusions to combat severe anemia.
3. Enhancing Quality of Life
Anemia and splenomegaly can contribute to fatigue, delayed development in children, and repeated infections; by correcting its root cause through BMT therapy, quality of life and overall health improve significantly for patients.
4. Prevent Long-term Complications
Patients suffering from severe PKD are at increased risk for complications including gallstones, bone deformities, and extramedullary hematopoiesis (an abnormal blood cell production outside the bone marrow). By treating their disease through BMT they can prevent these long-term issues. Get your screening done so you do not risk the life of your offspring.
Risks and Challenges of Bone Marrow Transplantation
While BMT may offer considerable potential advantages, transplantation should only be undertaken after careful consideration and due to specific considerations before being conducted.
1. Select an Appropriate Donor
BMT cases face one of its topmost obstacles in changing suitable donors- generally, sibling donors with matching Human leukocyte antigen( HLA) types are best, though unconnected donors could present lesser transplant complications and should thus be used where available.
2. Threat Factors of Graft- Versus- Host Disease( GVHD)
GVHD occurs when scattered patron cells attack a philanthropist’s body, from mild to severe conditions affecting skin rashes, liver dysfunction, and digestive issues to more serious issues that bear immunosuppressive drugs to manage. Unfortunately, these drugs also increase your risk of infections.
3. High Mortality Risk Related to Treatment-Related Therapies
The procedure involves intensive chemotherapy or radiation to eradicate diseased bone marrow before implanting new stem cells, rendering patients highly vulnerable to infections; potentially fatal transplant-related complications could also arise as a result of this conditioning regimen.
4. Failure Potential of Transplant
Sometimes donor stem cells fail to engraft with recipient bone marrow; this results in transplant failure requiring either another transplant attempt or alternative treatments such as immunosuppression and/or chemotherapy treatments.
5. Long Recovery Period
Recovery after bone marrow transplant can take months or years for patients’ immune systems to fully recuperate; during that period they are at increased risk of infections and complications. People tend to face deficiency disease of fat which also puts them at risk.
6. Side Effects of Chemotherapy and Radiation Treatments
Pre-transplant exertion procedures may beget nausea, hair loss, mouth blisters, and gravidity for some donors, with long-term consequences including secondary cancers or organ damage possible in rare cases.
Who Is Eligible for Bone Marrow Transplantation?
Not all PKD cases need or qualify for bone marrow transplantation( BMT). Deliberating over BMT depends upon multiple considerations, including;
- Anemia severity and transfusion dependence.
- Life-threatening complications (e.g., severe iron overload) must also be present for serious risk to exist.
- Your success as an organ transplant depends on finding a compatible donor.
- Overall health and ability to tolerate procedures
BMT may be considered a last resort option in patients suffering from severe PKD who have exhausted other methods for managing chronic hemolysis and face significant health risks as a result.
Alternative and Emerging Treatment Solutions
Other treatments are being investigated for patients not eligible for BMT transplants. Gene therapy offers hope of correcting their own cells’ mutation of PKLR gene mutation.
Conclusion
Bone Marrow Transplant (BMT) can offer hope to those suffering from pyruvate kinase deficiency; however, its risks should not be taken lightly. Research into alternative treatments offers hope to those unable to undergo transplantation for managing PKD better in the future.