Monitoring and Management of Chronic Complications of Pyruvate Kinase Deficiency
Monitoring and Management of Chronic Complications of Pyruvate Kinase Deficiency
Who is affected: Adults and children with PK deficiency
Why it matters:
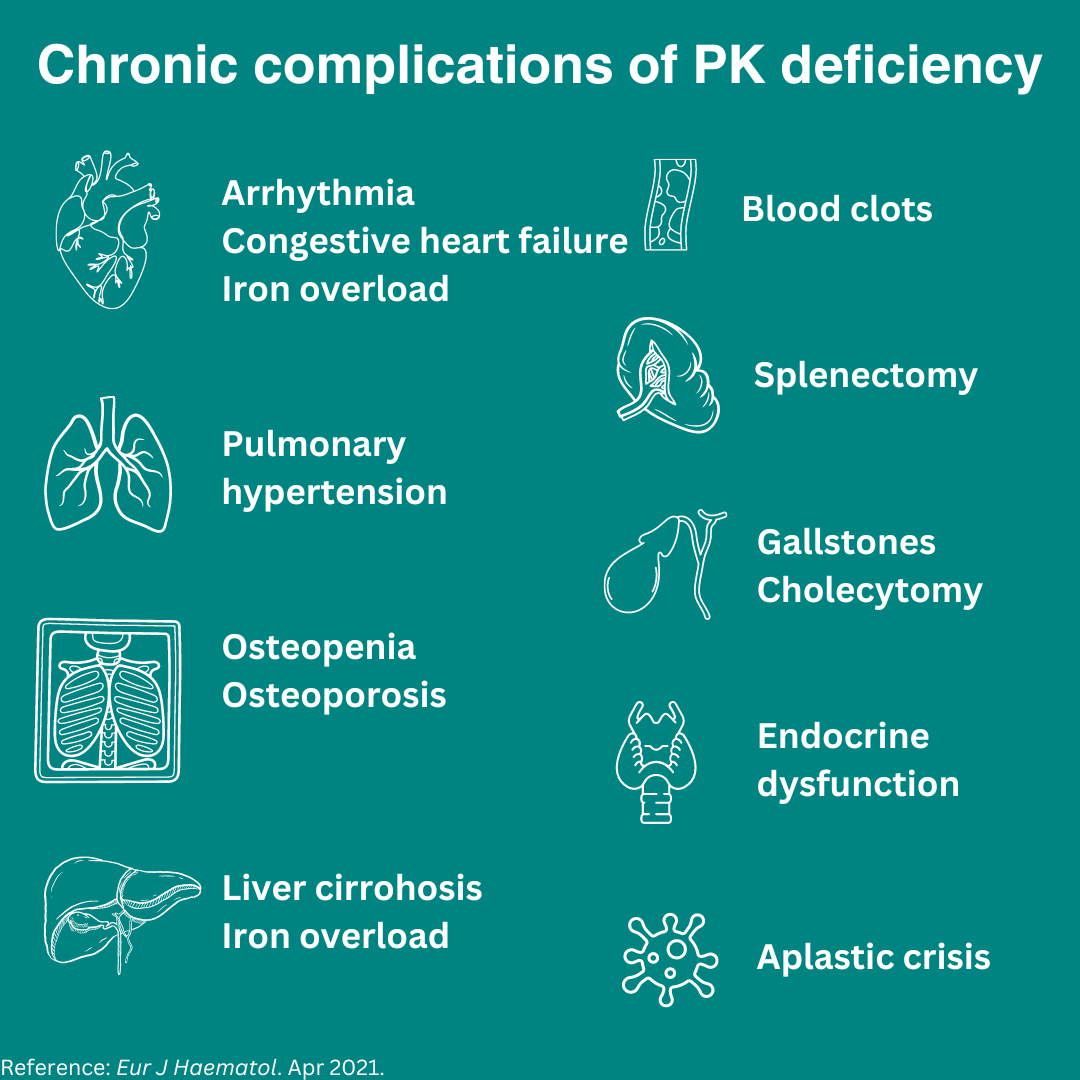
PK deficiency may result in a wide range of chronic complications, including iron overload, bone mineral density disease, heart and lung disease, and other problems. This happens even in people with PK deficiency that don’t have regular blood transfusions, making it important for all people with PKD to be regularly monitored for secondary health conditions.
Who is responsible for monitoring and managing PK deficiency and its symptoms?
- People with PK deficiency have a wide variability in the expression of anemia, symptoms, and disease progression.
- Ideally, people with PK deficiency will have a multi-disciplinary team including a primary care doctor along with a hematologist. Additional team members may include endocrinologists, cardiologists, pulmonologists, gastroenterologists, geneticists, infusion centers, dentists, nurses, social workers, among other clinicians.
- Hematologists monitor blood disease-related conditions but need the assistance of specialists for other chronic conditions.
- Pediatricians and primary doctors monitor and identify changes in growth and disease. They too need specialists to assist in the management of patients’ chronic conditions.
- If you’re having difficulty managing your health condition, seek help from a social worker, PK deficiency nonprofit group, family, or friend.
Guideline recommendations:
Screening Guidelines for Adults and Children with PK Deficiency
Condition
Measure
Iron overload
Measure ferritin:
- In adults and children (starting at age 3 years) or after 12 transfusions, whichever comes first, at least once a year
- RBC-transfused patients should be assessed every 1-3 months
Liver iron overload
Measure liver iron concentration (LIC) using (T2, T2*, R2, R2*) MRI
- In adults and children with ferritin >500 ng/mL (regardless of transfusion status)
- In regularly transfused or undergoing chelation therapy, annual liver MRI
- Non-regularly transfused, liver MRI at least once every 5 years and follow ferritin trends
- Non-transfused young children, first MRI after 5 years of age
Cardiac iron overload
Measure cardiac iron measurement using cardiac T2* MRI assessment:
- All patients with LIC > 7 mg/g dry weight
- Children should have their first cardiac T2* at 10 years of age if not regularly transfused or well transfused and well chelated
- In regularly transfused patients, monitoring is recommended yearly if high LIC or ineffective chelation; or 2 years if LIC is in target range and effectively chelated
Pulmonary hypertension
Screen with echocardiography in all patients 18 years or older every one to five years based on individual risk factors such as symptoms, prior ECG measurements, and history of splenectomy
Bone density loss
25-hydroxy vitamin D measurement:
Screen with echocardiography in all patients 18 years or older every one to five years based on individual risk factors such as symptoms, prior ECG measurements, and history of splenectomy
Bone density loss
Dual-energy x-ray absorptiometry (DEXA) scan:
- All patients beginning at age 18 years
- Further DEXA screenings should be based on the initial assessment
Thyroid, pancreatic, pituitary dysfunction
Endocrine monitoring:
- Patients with iron overload defined as serum ferritin >1000 ng/mL or LIC >5 mg/g dry weight.
- Hemoglobin A1c measurements are unreliable in hemolytic anemia and alternatives should be used to test for diabetes
Renal dysfunction
Renal function:
- In children and adults, irrespective of transfusion status
Chelation guidelines:
Iron chelation therapy is the use of medication to remove excess iron from the body. The PK Guidelines recommend chelation therapy in patients with PK deficiency age 2 years or older:
- LIC exceeding 5 mg/g regardless of transfusion status; and/or who have received 12 or more transfusions, or have a ferritin > 1000 ng/ml
Bottom line:
Adults and children with PK deficiency should undergo routine monitoring regardless of their symptoms or transfusion status, which can best be managed by a hematologist or well-trained physician that follows the International Guidelines for the Diagnosis and Management of PK deficiency.
