Pyruvate kinase deficiency (PKD) is a rare genetic disorder affecting red blood cells, often leading to anemia in children and adults alike. This hereditary condition primarily impacts how red blood cells generate energy, causing chronic hemolysis (the destruction of red blood cells). Given PKD’s rarity and complexity, international experts have formulated guidelines to improve diagnosis and management, supporting both healthcare providers and families in understanding this unique condition.
PKD can present symptoms that vary widely in severity, making diagnosis challenging. Early identification of symptoms such as chronic fatigue, jaundice, and splenomegaly (enlarged spleen) is crucial to improving patient outcomes. The following sections explore the nature of PKD, its symptoms, diagnosis, and treatment options, providing a comprehensive understanding of this condition and the best practices for managing it.
Understanding Pyruvate Kinase Deficiency
Pyruvate kinase deficiency is an autosomal recessive disorder, meaning both parents must carry the mutated gene for the child to inherit the disease. This mutation impacts the pyruvate kinase enzyme in red blood cells, which is essential for energy production. Without sufficient pyruvate kinase, red blood cells break down prematurely, leading to hemolytic anemia. Patients may require lifelong care and regular medical check-ups to monitor their red blood cell counts and manage anemia.
Symptoms of PKD
The symptoms of pyruvate kinase deficiency vary greatly, depending on the individual and the extent of the enzyme deficiency. Common symptoms include chronic fatigue, weakness, and pallor, all of which are associated with anemia. Some patients experience jaundice due to high bilirubin levels released during red blood cell breakdown. Children with PKD often show signs of slow growth and delayed physical development.
Other common symptoms include splenomegaly, which can cause pain or discomfort in the upper left abdomen. Gallstones are also common, as the breakdown of red blood cells releases excess bilirubin that contributes to gallstone formation. As children grow, they may experience delayed motor skills or physical abilities due to chronic anemia.
Due to the varied nature of these symptoms, early diagnosis is essential. Parents should be vigilant in monitoring any unexplained fatigue, jaundice, or abdominal discomfort in their children, particularly if there is a family history of PKD.
Diagnosing PKD
Diagnosing pyruvate kinase deficiency can be challenging, as its symptoms often resemble those of other hemolytic anemias. The diagnostic process typically begins with a thorough physical examination and a review of family medical history, followed by blood tests to assess red blood cell count and bilirubin levels. Doctors may also use a blood smear test to detect any abnormalities in red blood cell shape or size.
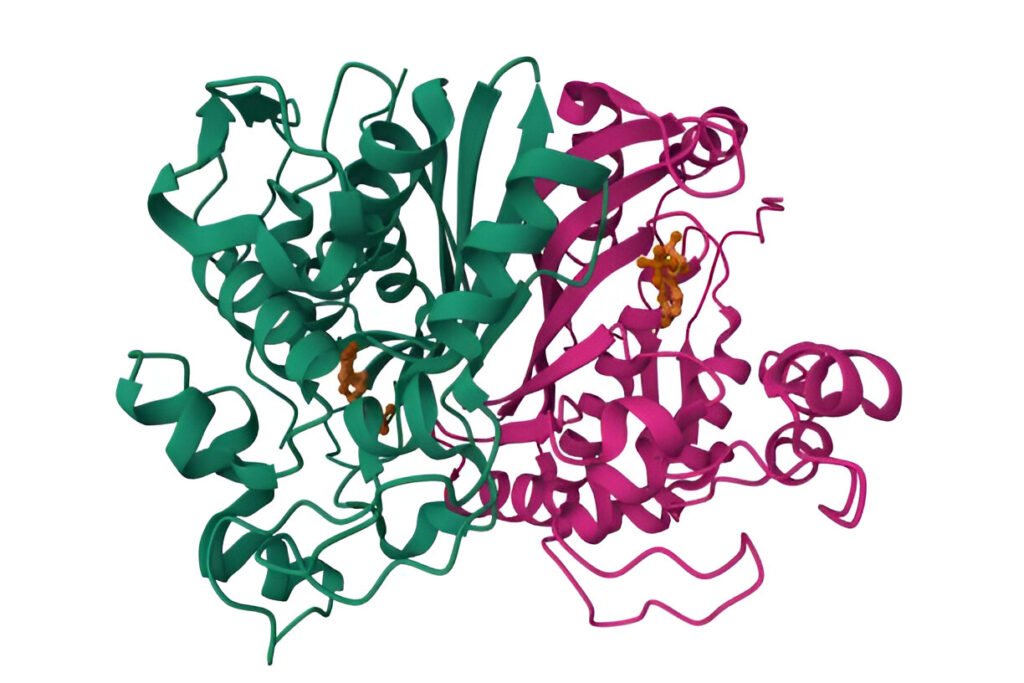
The key diagnostic test for PKD is an enzyme assay, which measures pyruvate kinase levels in the blood. This assay helps confirm a PKD diagnosis, differentiating it from other types of anemia. In some cases, genetic testing is recommended, particularly for families with a known history of PKD, to identify mutations in the PKLR gene that cause the deficiency.
Genetic counseling is also an important part of the diagnostic process for families considering future pregnancies. For parents of children health with PKD who carry the PKLR mutation, genetic counseling can provide information on the likelihood of passing PKD to their children and discuss any options available to manage this risk.
Treatment and Management Options
Managing pyruvate kinase deficiency symptoms, anemia, and treatment services deficiency involves a multifaceted approach, as there is currently no cure for PKD. Treatment primarily focuses on alleviating symptoms, maintaining red blood cell counts, and preventing complications. The course of treatment is tailored to the severity of the patient’s anemia and overall health condition.
- Blood Transfusions: For patients with severe anemia, regular blood transfusions may be necessary to maintain adequate red blood cell counts. These transfusions help reduce fatigue and support normal physical development, particularly in children. However, long-term transfusions can lead to iron overload, necessitating additional treatments to remove excess iron from the body.
- Splenectomy: In severe cases, doctors may recommend removing the spleen, a procedure known as splenectomy. The spleen’s role in removing old or damaged red blood cells can exacerbate anemia in PKD patients. By removing the spleen, the destruction of red blood cells is reduced, alleviating symptoms. However, splenectomy carries risks, such as increased susceptibility to infections, which is why it is typically reserved for patients with severe symptoms.
- Iron Chelation Therapy: For patients who require frequent blood transfusions, iron chelation therapy may be necessary to prevent iron overload. Excessive iron levels can damage organs such as the heart and liver, so removing the excess iron is crucial.
- Folic Acid Supplements: PKD patients often benefit from folic acid supplements, which support red blood cell production. Folic acid is essential for DNA synthesis, and supplementation helps the body produce new red blood cells to replace those destroyed by the deficiency.
- Monitoring and Preventative Care: Routine monitoring is essential for PKD patients to manage their condition effectively. Regular blood tests help track red blood cell counts and detect any complications early.
- Gene Therapy: Although gene therapy is still in the research phase, it holds promise as a future treatment option. Experimental studies aim to correct the genetic mutation responsible for PKD, potentially offering a long-term solution. While still in development, gene therapy could provide a viable treatment for PKD in the coming years, offering hope for patients and families.
Lifestyle and Support for PKD Patients
In addition to medical treatments, lifestyle changes can significantly improve the quality of life for individuals with PKD. Patients are encouraged to maintain a balanced diet rich in iron-binding foods and to avoid alcohol, as it can exacerbate symptoms. Exercise, though beneficial, should be tailored to the individual’s energy levels and monitored closely.
Support groups and counseling can also be valuable resources for families navigating the challenges of PKD. Organizations focused on rare diseases often provide support networks and resources, helping families connect with others who share similar experiences. This network can provide a sense of community and empower families to advocate for their loved ones.
Future Directions in PKD Research
The future of PKD treatment is promising, with research efforts focused on innovative therapies and improved management strategies. Gene therapy, in particular, offers hope as it targets the root cause of the disorder. Additionally, advances in hematology have led to the development of targeted therapies that may alleviate symptoms without the need for invasive treatments.
Research in PKD also extends to better diagnostic methods. With improved genetic testing and a deeper understanding of the PKLR gene, doctors may be able to diagnose PKD earlier, leading to better outcomes. Families affected by PKD should stay informed about these advancements, as they may lead to new treatment options shortly.
Conclusion
Pyruvate kinase deficiency (PKD) is a rare yet impactful genetic disorder requiring careful diagnosis and tailored management. Although there is no cure, treatments such as blood transfusions, splenectomy, and iron chelation can improve symptoms and quality of life for PKD patients. By staying informed and exploring ongoing research, families and healthcare providers can collaborate effectively to manage PKD, offering hope and support for those affected by this challenging condition.