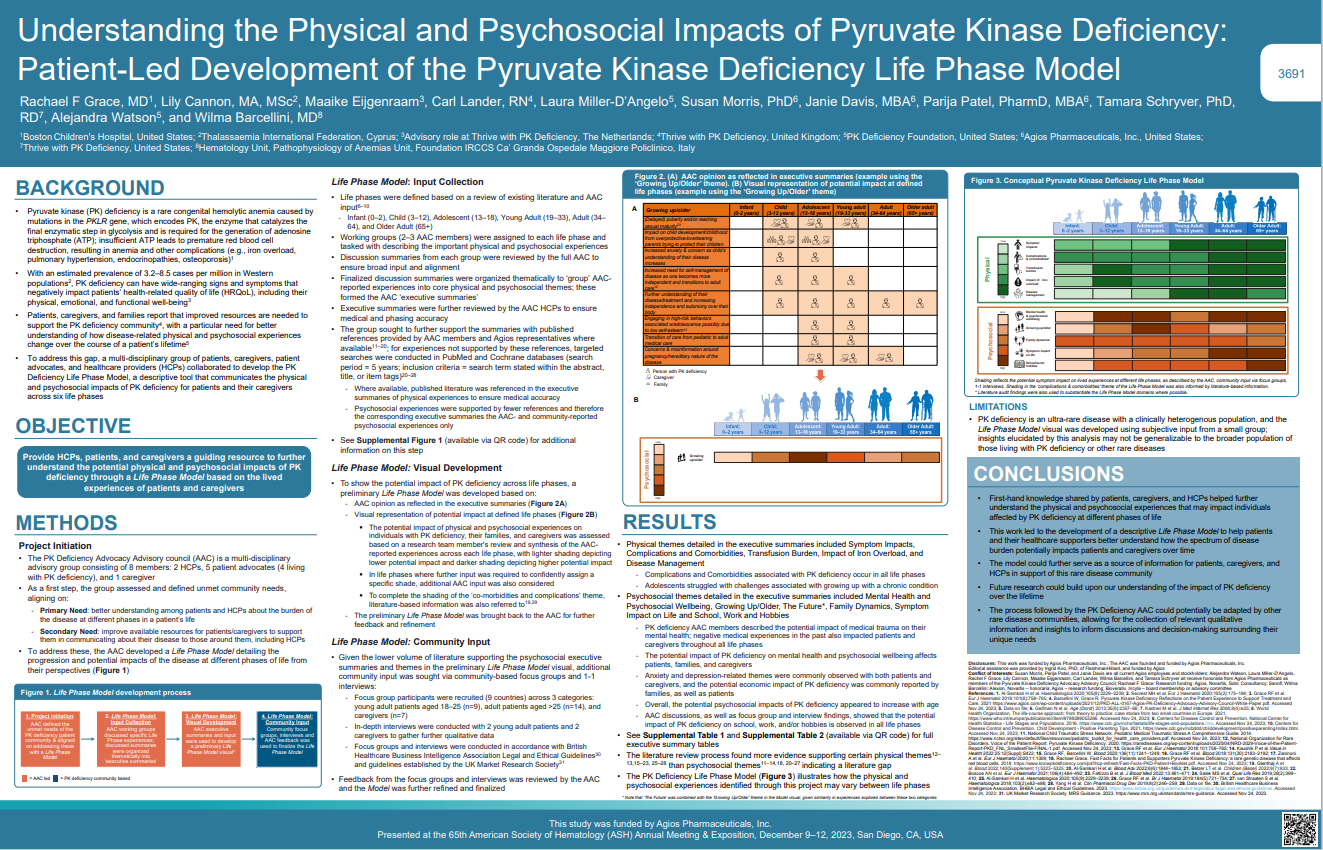
PK Deficiency Life Phase Model
People living with PK deficiency, their caregivers and families report that living with PK deficiency negatively impacts the person with PKD’s quality of life including their physical, emotional, and functional well-being. Improved resources are needed to support the PK deficiency community, with a need for better understanding of how the disease-related physical and psychosocial experiences change over the course of the affected person’s lifetime.
To address this gap, a group of patients, caregivers, patient advocates, and healthcare providers worked together to develop the PK Deficiency Life Phase Model, a descriptive tool that communicates the physical and psychosocial impacts of PK deficiency for patients and their caregivers across the six life phases:
- infancy (0-2 years)
- childhood (3-12 years)
- adolescent (13-18 years)
- young adult (19-33 years)
- adult (34-64 years)
- older adult (65 years+)
The project included the development of a model based on available research and fleshing out of life stages based on committee member experience. This information was converted to a visual model that was tested and refined within the PK deficiency community. The model was featured as an abstract at the National Organization of Rare Diseases (NORD 2023) and American Society of Hematology (ASH 2023) conferences.
The results of the project determined that:
- Complications and comorbidities associated with PK deficiency occur in all life phases.
- Adolescents struggled with challenges associated with growing up with a chronic condition.
- PK deficiency Advocacy Advisory Council* (AAC) members described the potential impact of medical trauma on their mental health; negative medical experiences in the past also impacted patients and caregivers throughout all life phases.
- The potential impact of PK deficiency on mental health and psychosocial wellbeing affects patients, families, and caregivers.
- Anxiety and depression-related themes were commonly observed with both patients and caregivers, and the potential economic impact of PK deficiency was commonly reported by families, as well as patients.
- Overall, the potential psychosocial impacts of PK deficiency appeared to increase with age.
- AAC discussions, as well as focus group and interview findings, showed that the potential impact of PK deficiency on school, work, and/or hobbies is observed in all life phases.
- The literature review process found more evidence supporting certain physical themes than psychosocial themes indicating a literature gap.
- The PK Deficiency Life Phase Model illustrates how the physical and psychosocial experiences identified through this project may vary between life phases.
If you are interested in pursuing a project with the Life Phase Model, please contact a member of AAC; [email protected], [email protected] or [email protected].
*Funded by Agios Pharmaceuticals Inc.
Patient Stories
Jullie Reaser, Patient
California, USA
My name is Julie Reaser and I’m 55 years old. I was diagnosed with PK deficiency in high school when I attempted to donate blood at blood drive and learned my hemoglobin was too low. My parents took me to a local hospital where blood tests were run but the doctor was unable to identify if anything was wrong. I was then referred to a specialist in San Diego, CA, where a diagnosis of pyruvate kinase deficiency was made. As part of my treatment, my spleen and gallbladder were removed.
I depend on red blood cell transfusions when I feel symptomatic, which includes exhaustion, brain fog, and joint pain. I get blood transfusions every other month. I'm on chelation therapy for iron overload and I get annual scans of my heart and liver to measure the effectiveness of chelation. As I’ve gotten older, I’ve started to experience other side effects of iron overload like pre-diabetes, arthritis, and osteoporosis. Last year I had a serious hip fracture that required pins to stabilize my bones.
I believe guidelines for the treatment of PK deficiency are vital and it starts with a knowledgeable hematologist, which is difficult to find. Now that I have found mine, I feel like my well-being is a priority and I have regular appointments with him to discuss treatment, symptoms and medication. I trust his decision making regarding my health considering all the ways PKD can affect the body and quality of life.
In my free time, I enjoy reading, spending time with my daughter and granddaughter, and going out to eat with my mom and sister. Thank you for reading my story!


Emma Marsh, Carer, and Daughter, Maisie, Patient
Liverpool, Great Britain
Maisie is my 16 year old daughter who was born with pyruvate kinase deficiency. Three hours after birth she received a red blood cell transfusion and to date, has received 110 transfusions. We didn’t receive a diagnosis until she was 14 months old despite her having blood transfusions every four weeks from birth. When she was five years old she had her spleen removed and her hemoglobin stabilized allowing a pause in her blood transfusions until her teen years. Maisie now has transfusions whenever she becomes unwell (or experiences symptoms of PKD).
She had a long intravenous line in her leg that delivered blood at ten weeks old, which she managed to kick out herself, a Hickman line which become blocked after a week, and two port-a-caths, which were supposed to provide easier access to her veins. She is currently waiting for her ferriscan results as her ferritin levels have been very high.
As a mother, I think the guidelines for care are important because this disorder is very rare and not many people know about it, including doctors and consultants we’ve meant in general practice. Maisie misses a lot of school and I’ve received emails from education and local authorities regarding her attendance as her condition is unknown and the severity is hard to describe. More information is needed to raise awareness of those with PKD and how it impacts their lives.
Treating PKD is different for each affected person. Maisie now only needs blood transfusions when she is unwell from viruses, which may be once or twice a year. Before her splenectomy, she received blood every three to four weeks. Life is very limited for those living with PKD and more research is needed to find something that will not only ease the symptoms cure this illness.
Maisie is a homebody. She loves being at home with myself, her dad, her two sisters, Ruby and Scarlett, and her Beagle dog Bear. She is currently working on her General Certificate of Secondary Education and we are planning her Leavers prom. She is hoping to go to college to study hair and beauty in September. Maisie is generally a very kind, caring, and happy girl.
Cathy Miller, Patient
Greenville, Pennsylvania
My name is Cathy Miller, and I was born with PK deficiency. Because I had a cousin born with PK deficiency a few years prior the doctors knew what life sustaining measures to implement. I was treated with phototherapy and an exchange transfusion, followed by a series of regular red blood cell transfusions until age 5, when I had my splenectomy. After that I was transfusion free.
At age seven, and at age 18, I had a tonsilectomy after much confusion about the unusual symptoms. A liver biopsy during surgery indicated cirrhosis of the liver. It was strongly hinted that I abused alcohol, which was incorrect because I'm a nondrinker.
Because my family relocated when I was six months old, there was some confusion about the original diagnosis and my pediatrician indicated I had spherocytosis. In 2012 I asked for genetic testing which confirmed PK deficiency.
Without any formal education about red cell morphology, I was the first to point out my macrocytic red cells and elevated reticulocyte count were not consistent with spherocytosis or CDA type 11 as one hematologist suggested. I was told PK deficiency was only seen in textbooks, and because I had already had a splenectomy, no further treatment was available. I was also told the only way to get a definite diagnosis was to do a bone marrow biopsy and they assured me I didn’t want to do that.

Now in 2024 I have osteoporosis, cardiac valve abnormality, liver scarring, low hemoglobin, exercise intolerance, and fatigue. However, I’m reassured at my annual visits to my hematologist that my numbers are good even if I don’t feel well and there’s no need for further treatment. I had an MRI seven years ago to test my liver iron content and was reassured I don’t need to repeat that if I’m transfusion free.
I was excited to participate in the mitapivat drug trials, but unfortunately, I had no response to the medication even though other people with PKD do.
I am looking forward to the change in guidelines for PKD patients addressing the whole person and all their unique needs. Sometimes I don’t know what to fight for and what to let go of and accept.
People with PKD needs are multi-tiered and should be addressed to bring the best quality of life to the patient. These needs vary by age and circumstance. We need hematologists who are willing to address all the complications associated with the disorder rather than focus on hemoglobin levels only. It needs to be understood that when a patient with PK deficiency is sick, they are very sick. A fever is an emergency that needs to be addressed immediately, especially if the person has been splenectomized. Identifying the source of the fever is critical, which not all emergency departments understand.
I have hopes that with all the recent research, our babies born with PK deficiency will be diagnosed quickly and will have multiple options available for treatment. I’m hoping their lives will be as close to normal as possible. Living with PK deficiency is difficult without all the added stress of not being understood and heard. My wish is for medical professionals to be well educated on the challenges of living with PKD and to take our disease seriously.

Bosch-Nuvelstijn Family
Netherlands
We are Mariska Bosch and Martin Nuvelstijn, parents of Tess (11 years old) and Lisa (6 years), from the Netherlands. Both of our daughters were born with pyruvate kinase deficiency.
Tess weighed 2520 grams (5.6 lbs) at birth and had a lot of difficulty emptying her bottles. When she was six weeks old, her blood was taken, and it turned out that she had an hemoglobin of 2.3 mmol/l (3.7 g/dL). She then received her first blood transfusion. Her hemoglobin was tested every 2 weeks. She is now 11 years old and has undergone a total of 56 blood transfusions.
Lisa weighed 2820 grams (6.2 lbs) at birth. A chorionic villus test was taken during the pregnancy, and it showed that she also had PKD. Lisa immediately had to undergo blue light therapy due to her high bilirubin and was tube-fed for the first three weeks. Lisa is now 6 years old and has undergone a total of 59 transfusions.
At the age of 2, Tess her spleen was removed, and her transfusion period then increased from every 4 weeks to every 10 to 12 weeks. Lisa was a fussy baby and spent a lot of time in the baby carrier. Her transfusion period is every 5 to 6 weeks.
We are currently being treated by a pediatric hematologist at the Utrecht Medical Centre.
Both our daughters are active girls; they like to swim, dance, and be with friends. They are completely in love with our two main coon cats: Nala and Sifa.
The guidelines for diagnosing and treating PK deficiency, will be enormously helpful. Fortunately, there is much more information available about pyruvate kinase deficiency than there was 11 years ago. The sooner the guidelines will be integrated in hospitals, the better it will be for diagnosis. It will take away some of the uncertainties from the beginning.